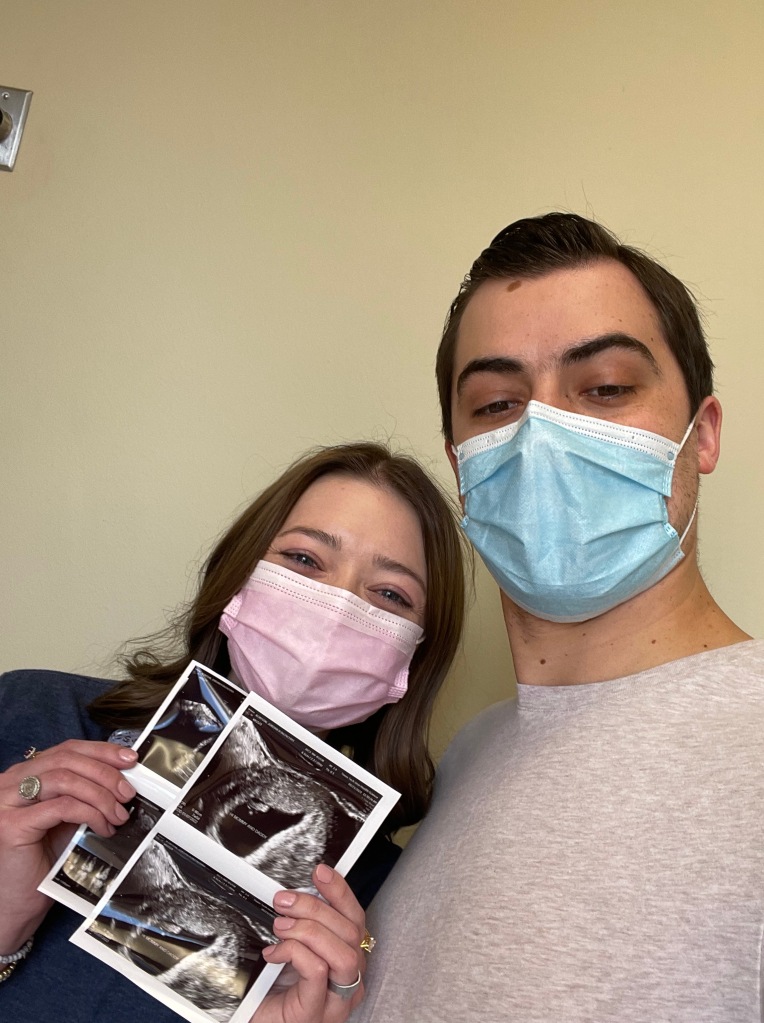
It’s been over a year since I have written. That doesn’t seem possible, but I guess having a newborn, and now, a toddler, will do that! Cohen is almost 16 months old, which means it has been 15 months since we left the NICU.
If you’ve read his birth story, you know he was born at 34 weeks and 4 days because he had Intra-Uterine Growth Restriction (IUGR) and was born 2lbs 11 oz. The tiniest little babe! I have wanted to write about our time spent in the NICU, but honestly, just couldn’t bring myself to do it until now. Unless your own child has spent time in the NICU, you don’t know what a traumatic experience it can be. And even though we knew ahead of time that Cohen would be born early and would be in the NICU, I don’t think there was anything we could have done that would have prepared us for the worst month of our lives.
Thinking about Cohen being in the NICU, walking past the NICU at work, and even looking at pictures from that time, makes me nauseated. I think I have a small amount of undiagnosed PTSD.There is probably a lot I will leave out – unintentionally – because it has been so long, or possibly because I blocked it out. Thankfully, the NICU gifted us with a “NICU Diary” our first day. I kept up with it until I started back to work 2 weeks postpartum (yes, I was crazy), and then life was too hectic! But, I will do my best to share all of the details, because that’s what I do best. I think details are important, but more than that, I think the details in this story will show you the faithfulness of God – that even in those deep, deep valleys – He is there, and He alone is our strength. So, join me in recounting the hardest, most trying time I have ever been through. And truly, I think that is saying a lot, considering what I have lived with and through.
Cohen’s Birthday
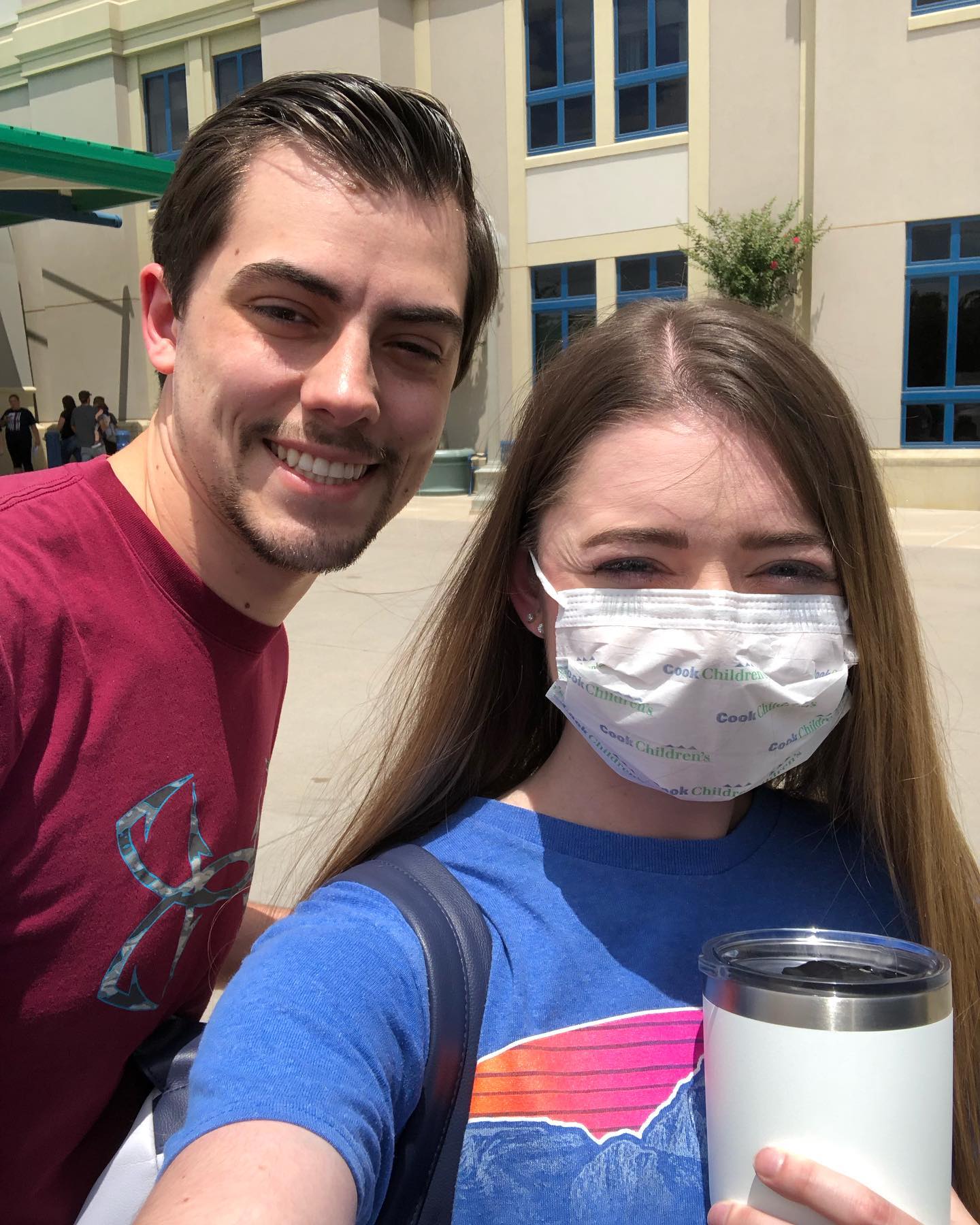
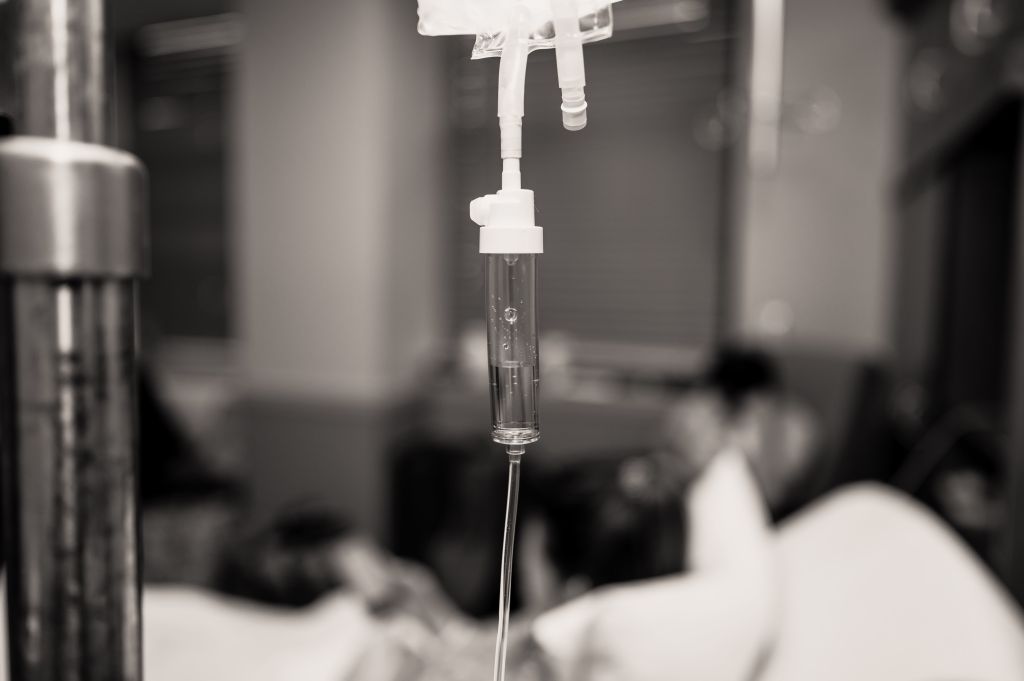
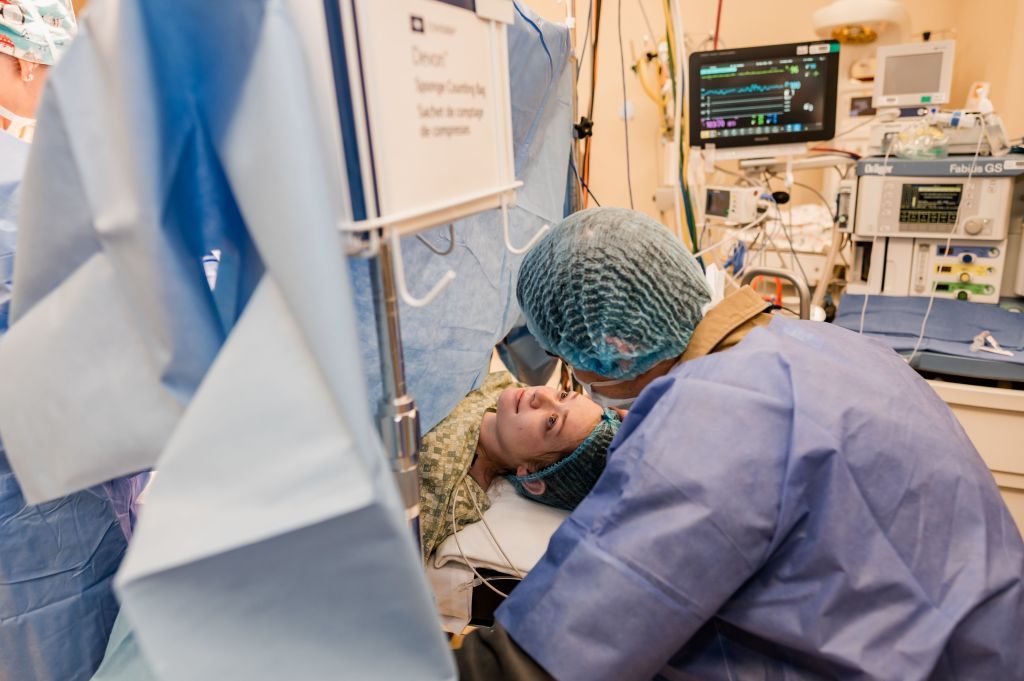
Our first day in the NICU was a whirlwind. Cohen was born at 6:10AM and was taken straight to the NICU. Jason went with him and was able to hold Cohen’s finger before he was told he couldn’t stay, and was led back to the OR where I was. Once we were out of the OR, I was led back to my room in the family birth center to rest. I’m not sure how long we were in there, but within the hour, my nurse brought me a hospital pump so I could begin pumping breastmilk. I was expecting this, thankfully. Not much later, we were taken to the family care unit where I would be for the entirety of my stay.



Around noon, I could finally feel my legs, so I felt well enough to get into a wheelchair so we could go to the NICU and see Cohen. It had been six hours since I had seen my baby. We stopped at the front desk of the NICU and checked in, then were instructed to sanitize our phones and to wash our hands well. We did all of this every singly time we came to see Cohen. We were led to a “pod” (room where each baby was separated by walls on each side, with a curtain that you could close off to give you privacy), and Jason pointed Cohen out to me – the first baby we came across. I immediately started crying. He was so tiny. He lay in his isolette, eyes closed, with a nasal cannula in his nose to provide oxygen and an oral gastric tube in his mouth. He had parental nutrition line in his belly button and leads keeping track of his heart beat. He might have had a few other things attached, but that’s all I can remember/see in pictures. Our nurse, Gaye, came up to us and explained Touch Times – these were designated times when we were allowed to hold and feed Cohen. At each touch time, we washed our hands, took Cohen’s temperature (had to make sure he was staying warm!), changed his diaper, fed him and held him. Because rest is so important for little babies, we had to make sure we didn’t hold him outside of those times so he could grow and stay well. Unfortunately, we had not shown up at a designated touch time (we didn’t know), so I wasn’t allowed to hold Cohen yet. Our nurse was so sweet and understanding, and she knew how difficult this was, so we were allowed to open the side doors of the isolette and touch Cohen while he slept. We FaceTimed both my parents and Jason’s parents so they could see him as well.


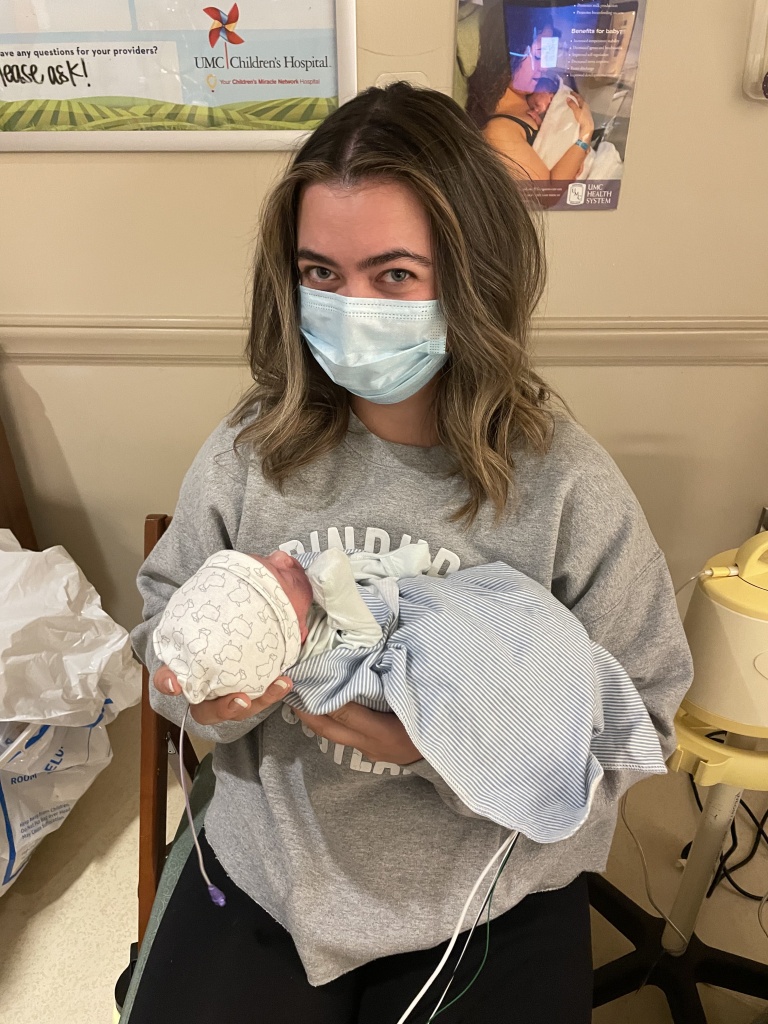
Cohen’s touch times were 8am, 2pm, 8pm and 2 am that first day, but when we came, we would stay for hours. So, I finally got to hold my baby after the 2pm touch time because he was doing SO well (according to the time stamp on the photo, it was close to 5PM when I finally got to hold him – almost 11 hours later!) By that time, he had been taken off of oxygen completely and was breathing on his own. We stayed until my pain meds were wearing off and I needed to eat and pump. While we went back to the room, my parents got to go to the NICU and see Cohen.

Later that evening, while Jason showered, I took Karli with me to the NICU and she got to take his temperature and watched as I changed his tiny little diaper. She got to hold his little finger while the nurse checked his blood sugar and he screamed and cried!

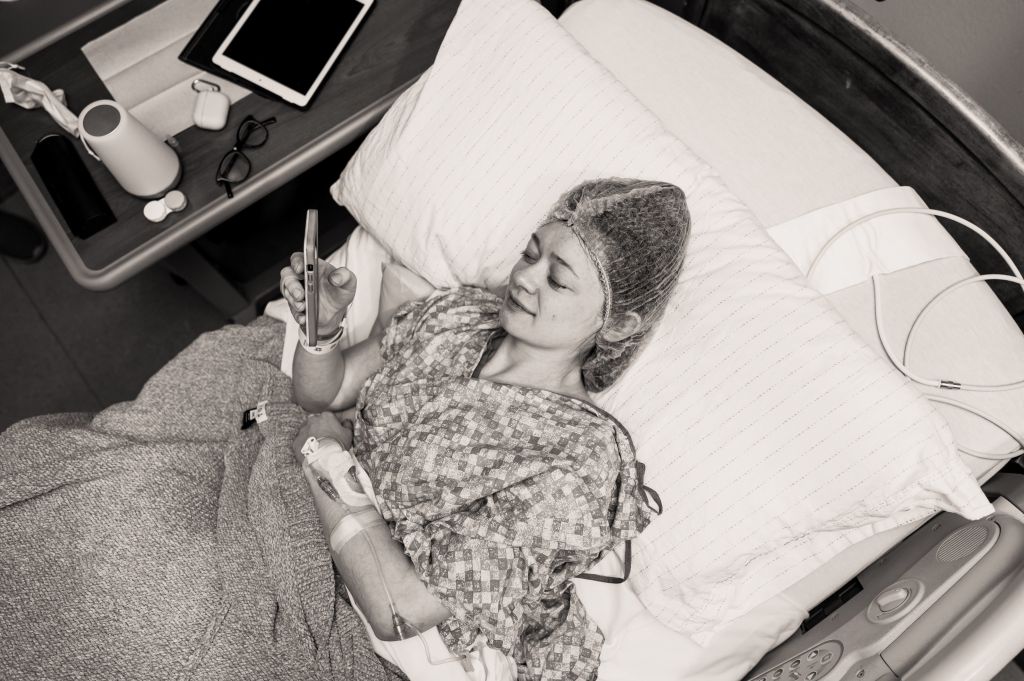
Throughout the night, Jason and I set alarms to get up every 3 hours so I could pump. What a night. Pumping was painful for me as it was causing my uterus to contract. Jason was so sweet to get up with me and help me with all of the supplies and pump parts. He washed every single pump part after every pumping session and helped me label colostrum and the small amounts of breastmilk I would get so we could bring it to the NICU for Cohen.
1 Day Old
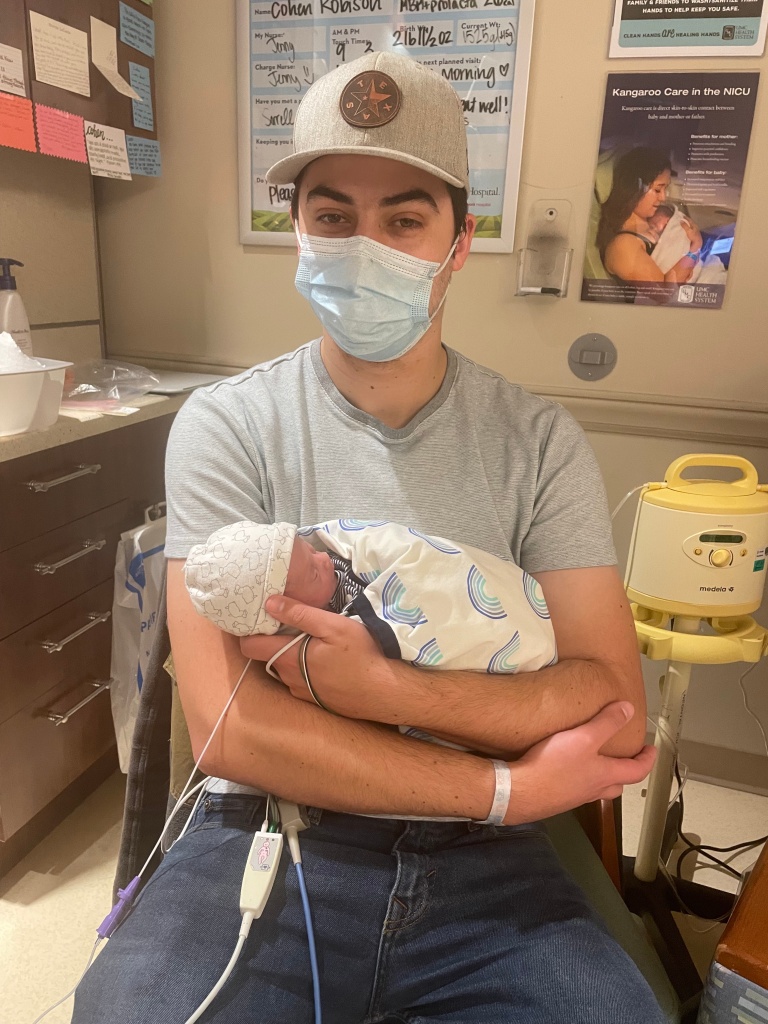
The next morning, we showed up to Cohen’s 8am touch time and Jason got to hold Cohen for the first time! We stayed for over an hour, taking turns holding our son. Cohen’s bilirubin levels came back high, so he had to be under the blue spectrum lights (also called phototherapy) for a day. He wore little “goggles” so the lights wouldn’t hurt his eyes, but we kept trying to pull them off. Jason’s mom got to come up to the hospital and see Cohen with Jason present, and Jason’s cousin, Jancee, got to come and see him as well. At Cohen’s 3PM touch time, we gave him his first bottle! I think it was 3 mls. He had to start off with very small amounts of breastmilk so his tummy didn’t get overwhelmed. At this point, we started off with 3mls every 6 hours. He was also still on parental nutrition at this time. We also started working on breastfeeding after his bottles this day, just for practice. Cohen’s mouth was so small, this would prove slightly difficult. We were encouraged to use a nipple shield to help him out, which we used up until I stopped nursing Cohen.



We were present when the doctors rounded on Cohen today as well – I did my best to be there every day for rounds. There were two teams – one team of neonatologists, and one team of nurse practitioners (NP). Cohen was on the NP team so we got to know each NP well and I grew to love each of them. But this day, for some reason the doctors rounded on Cohen. I won’t name names, but he didn’t have the best bedside manner. I asked what it would take to bring Cohen home and how long he expected us to be there (normal questions for a mama in the NICU, right?), and he responded as if I was asking some pretty dumb questions. I tried not to take it personally. He told us to expect to be in the NICU for 4-6 weeks and that Cohen would have to be at least 4 lbs to be able to sit safely in a carseat. So our biggest goal was for Cohen to reach 4 lbs and not have any issues. Then and there, I became obsessed with Cohen’s weight and all things “numbers” when it came to my baby.
Later that night, Cohen got his oral gastric tube removed and got first sponge bath. Cohen’s nurse that day was Kelsie, someone I had met many years ago, but hadn’t seen since. It was so special to have her as our nurse! She helped Jason give Cohen his sponge bath – I watched and took pictures since I was still in quite a bit of pain (the day after a c-section is definitely the worst) and still required the wheelchair. Cohen was PISSED. He cried the entire bath – his whole body turned a bright red from being so upset! It was kind of funny. His little cry sounded like squeaks. I took a video of it and now it saddens me to watch it 😦 But, once Jason started rubbing his head, he completely calmed down and went right to sleep. We soon learned that when we needed to calm Cohen down, rubbing his head was the answer!



We stayed well past midnight holding our baby and loving on him. We were so thankful to be spending so much time with him, even if we had to be a part a lot of the time.
2 Days Old
We were back at 8am for Cohen’s first touch time of the day. Cohen’s bilirubin levels had come down, so he was able to stop the phototherapy. Cohen had gained weight and was now 2 lbs 14 oz. He still remained on parenteral nutrition and fluids, but they increased the breastmilk amount to 6mls every 6 hours and Cohen devoured it every time. I took a video of Jason holding Cohen that morning while Cohen slept and had the cutest, squeakiest hiccups. Adorable! I love watching that video too, because in the background you can hear the nurses celebrating that another little baby drank 35 mls (~1 oz) and how excited they were for her! That’s just how it is in the NICU – you celebrate every single milestone, whether big or small. And honestly, looking back, 35mls seemed like so much at one time, lol.
Later this day, Yai-ya (my mom) got to come and hold Cohen for the first time, and she loved it, of course. Jason’s Dad (Papa J) also got to come and meet Cohen with Jason present while I ate dinner. After dinner, we spent the evening in the NICU holding Cohen. One of the lactation consultants started coming by to see me at least once a day to help Cohen and I with the breastfeeding process. She brought me a hospital pump to Cohen’s NICU room and I would pump at every touch time there so I didn’t have to be away from Cohen.


3 Days Old
Today, they started to swaddle Cohen (which he looooved) and he was able to start getting 3mls breastmilk every 3 hours now instead of every 6 hours. Swaddling Cohen in the isolette is something that doesn’t usually happen until a baby weighs a certain amount (can’t remember why this is or what the weight is), and Cohen didn’t weigh that amount yet. But, his nurse fought for him to be swaddled early because Cohen was constantly moving and kicking his legs, which meant he was burning off all of his calories that he needed to keep weight on. Once he was swaddled, he was much more calm!
We spent as much time as we could in the NICU this day because I knew I was getting discharged to go home. I had the best OB (Dr. Richards), and I think she let me stay an extra day because of our situation. We also had one of the best nurses this day, which actually turned out to be the sister of some of our dear friends! At one point, it was time for my pain medication, but I was in the NICU, so she walked it down to me so I wouldn’t have to leave! The best!! She made sure to tell me that I could be discharged whenever I was ready. We ended up leaving close to 9PM that night. I was completely heartbroken – leaving my baby behind while we went home. Sitting here typing this, I am in tears thinking about that night. I cried the entire drive home and for a majority of the night. We just kept telling ourselves that the NICU was the best place for you and that your nurses loved you so much!
Overnight, we continued our regular schedule of getting up every 3 hours for me to pump and Jason to clean parts. I had purchased a Willow pump because I wanted to be able to pump at work without issues, so that’s what I was trying to use at home. I *thought* I had done a lot of research before I bought that pump, but it turns out I had not done enough. The next several days were filled with me trying to figure out how to use that thing. I’ll spare you the details, but I eventually learned it’s not meant to be used as the primary pump!


4 Days Old
Cohen’s touch times changed to 9, 3, 6, 9 (AM and PM) this day, and that is what they stayed the rest of his stay. So we showed up at 9AM! Cohen had gained weight – 1310 grams ( we started going by NICU weights) and his feeds had been increased to 6 mls every 3 hours. He still had TPN and fluids. At this point, I was no longer using a wheelchair and could walk, but was still in quite a bit of pain. Jason became a pro at taking Cohen out of his isolette every touch time – maneuvering all the wires and IV pole – all while holding Cohen in one arm! The nurses would joke that Jason should become an honorary nurse. We learned how to do everything ourselves, and the nurses trusted us with that.
Jason and I knew that both he and I would be going back to work the next week, so we started figuring out a good schedule that allowed us to keep our sanity and still see Cohen as much as possible. While we were both still at home, we came to the 9 AM, 12 PM, 3PM touch times together. Then my mom would come with me to the 6 PM touch time. We decided it was too much for us to try and make it to the 9PM touch time, so my mom ended up going to that one every night. We weren’t allowed to have food in the NICU, so our usual schedule at each touch time went like this: Show up, wash our hands, check Cohen’s temperature, change his diaper, feed him (usually, I would pump while I fed Cohen or while Jason fed Cohen), snuggle Cohen for an hour and then head home. We did that every 3 hours. Yes, it was exhausting, but we couldn’t see another way.

This day, Cohen started to be a little more awake for us and would open his eyes. I started singing to him, and he would smile every time. It was the cutest!

5 Days Old
Cohen is 1315 grams! He slowly, but surely, gains a little weight every day. Praise! His feeds were increased to 10 mls every 3 hours and at first, he was enjoying it. Soon, he started to get too tired to drink all of his bottles. The nurses warned us that if that continued, he would have to have a nasogastric tube (NGT) placed. I was hoping that wouldn’t have to happen. Dad got to have kangaroo time with Cohen, which just means skin-to-skin. it was so sweet! We did a lot of snuggling while we watched Redeemer church online from the NICU. Cohen also had more visitors this day! Bess, Jason’s cousin and my sweet friend, got to meet Cohen and hold him this day. We started seeing a lot of Cohen’s personality start to come out in his cute little expressions.

Jason’s parents also got to hold Cohen for the first time this day. It was kind of by accident – they had showed up outside of a touch time to honor they time that Jason and I were spending with Cohen (only 2 people could be in the NICU at a time with each baby), and our nurse was kind enough to let them hold him. I was actually sad to learn that, because it was important to me that I was present for any family or friends to hold our baby, because it was so special! But I hadn’t told anyone that, so no one knew! I let it go pretty quickly, and was just thankful they got to hold him.


6 Days Old
This morning, I got a call from Cohen’s nurse that Cohen had to have an NG tube placed because he wasn’t drinking enough of his bottles. I was devastated! I knew it wasn’t the end of the world, but it still hurt my heart. Also this morning, my friend and birth photographer, Britney Looney, came with me to the first touch time. Jason started back to work today, and we didn’t have any birth pictures of me holding Cohen (since that didn’t happen when he was born), so she was sweet enough to come with me to the NICU and take photos of us there! Of course this was the day Cohen chose to have an NGT placed! So that was in all of our photos. But that’s okay! Looking back, that doesn’t bother me at all – it’s just part of the memories. Also, my dad (Pappy), held Cohen for the first time today.





7 Days Old
Cohen’s feeds went up to 17 mls every 3 hours. At every touch time, we would feed him what he wanted from the bottle, then the rest would go through his NGT. Cohen was starting to become more alert and for longer periods, so that was really fun! Cohen got an ultrasound of his spine and head today, which was just part of protocol. I had a small baby shower thrown for me by the dietitians this day, so I got to attend that in between touch times. They made a sweet banner with Cohen’s name on it that we hung on Cohen’s isolette. It was the perfect touch!


8 Days Old
Cohen’s feeds went up to 22mls every 3 hours and he started to fill out a little more! We started swaddling with our own blankets and using our little preemie hats, which was so fun! Jason’s mom was nice enough to drive me up to the hospital for the next couple of mornings since I still couldn’t drive and remained on pain meds, so she got to hold and snuggle Cohen quite a bit during our time there in the mornings. Jason would go me with at the 12 PM touch time and then I would usually go with my mom or a friend at the 3PM, then Jason and I would go to the 6PM together.

9 Days Old
I started back to work today. You may be wondering why I chose to go back so early. Since I was working part time, I didn’t get benefits, so I had no PTO/vacation days and I only got 6 weeks of paid leave. I used one week for Cohen’s birth, so I wanted to save all the time I could for when Cohen actually got to go home. I planned to still have 3 months off, but if I used that while Cohen was in the NICU, that would mean I would only get 2 months at home with him, which I knew wouldn’t be enough time! I guess the good thing about going back to work so early, was that the cancer center was just a short walk down the hall from the NICU! So I would show up every morning to Cohen’s 9AM touch time and do our usual routine, only now I was going by myself. It was SO hard. I would take Cohen’s temp, change his diaper, hook up to the pump, then bottle feed him while I pumped. We would snuggle (also while I pumped) while the rest of his feeds went through his NGT. I would usually stay about an hour, then head to work. I always tried to scarf some lunch down while I charted so that I could go to Cohen’s 12 PM touch time and do it all over again. Jason would meet me there, which helped a lot. I usually had a friend or my mom at the 3PM touch time, and then I would go home around 4:30. Jason and I would go the 6PM together, then go home to eat dinner and sleep. We did that every weekday for 3 weeks. It was hell. But, back to the good things!


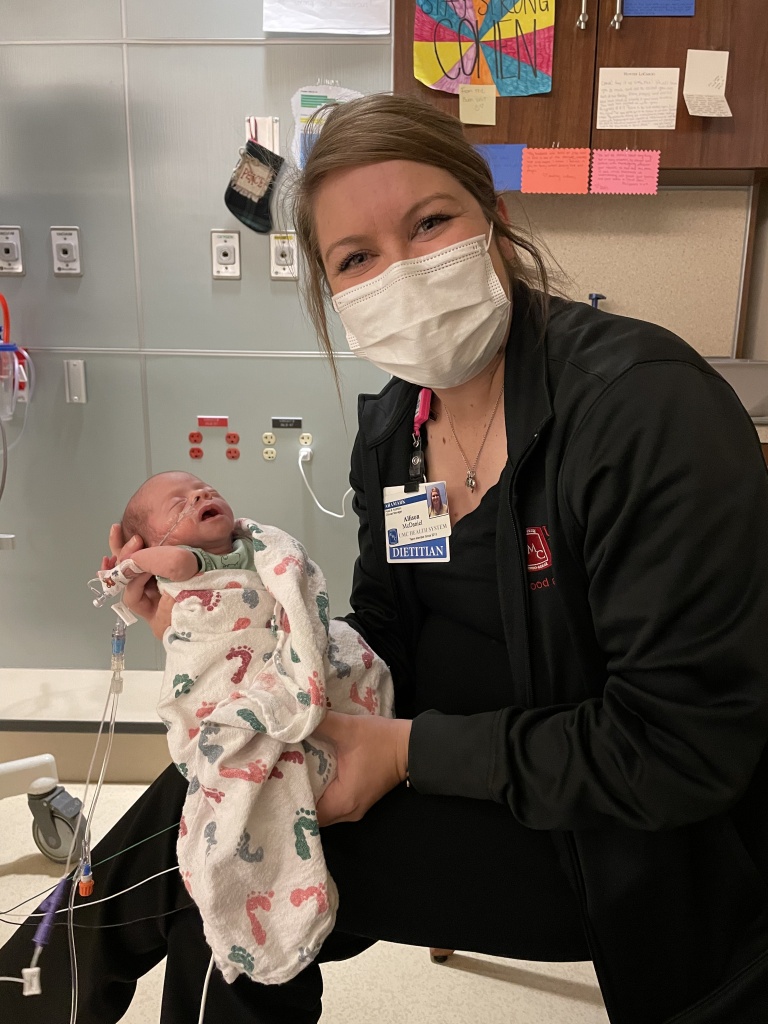
Cohen weighed 1500 grams this day, so he weighed enough to finally start wearing clothes! He barely fit into the preemie clothes we had, but it was the cutest! We started to notice his cheeks filling out more, too. My boss, Allison, had been out of town when Cohen was born. I was sad because she’s the NICU dietitian, so I had hoped she would be there while we were there! Thankfully, she supported me from afar, but she finally got to meet and hold Cohen this day! Jason’s cousin, Jaree, also got to meet and hold Cohen today! Another win, was that Cohen was starting to get better at breastfeeding. I started to nurse him at every touch time. If I remember correctly, it “counted” if he nursed at least 15 minutes. If it was any less than that, we still offered the bottle and then would put the rest through the NGT. This day, he nursed for 6 whole minutes!


10 Days Old
My best friend, Megan, got to meet Cohen today! Also it’s worth noting that I stopped writing in the NICU diary. It just got to be too much and I had forgotten all about it! At least I documented things on Instagram, lol. Cohen got moved to an open crib this day! This happens when they reach a certain weight and they can start to maintain their own body temperature a little better. I remember our nurse encouraged us to layer Cohen in two outfits, a hat and two swaddles so he wouldn’t “fail” and have to go back to an isolette. Thankfully, Cohen is warm-natured like his daddy and we only double-layered that one night!


11-15 Days Old
Jason and I learned about home delivery with HEB and what a GIFT that was!!
Karli held Cohen for the first time!
We dressed him in all the cute preemie clothes.
He started taking more and more breastmilk by mouth and was nursing longer!
During this time, Cohen started getting a bad diaper rash that we couldn’t get ride of. Us and the nurses were trying all of the creams!! We eventually gave him his first sitz bath (imagine a baby hot tub, basically) and he loved it!

16-20 Days Old
We had a rude nurse. I showed up to his 9AM touch time (which I had never missed) and he had already been bottle fed. I was crushed that I wouldn’t get to nurse my baby. The nurse that day was one we had not had before – she said that Cohen had been crying and was hungry, which is why she fed him early. Of course, I understood that. But it doesn’t mean I wasn’t still hurt and felt like I had missed out. That’s how I connected to my baby, whom I couldn’t live with yet. I asked if she would call me first if that happened again. She seemed agitated that I would ask this. Then she noticed my scrubs. I told her that if she called me, I could be in the NICU within 5 minutes. Thankfully, it never happened again.
My friend and coworker, Sam, got to meet Cohen this day! Unfortunately, while she was holding him, Cohen got a hold of his NGT and pulled it out. It was scary! When it happened, I was pumping, so I called to his nurse to let her know what happened. She was in the next room feeding another baby, so she told me to make sure the NGT was pulled all the way out so he wouldn’t choke on any of the breastmilk going through it at the time. I did as she asked. Sam left not too long after that, poor thing, lol. Before I left, I stayed and held Cohen while the (rude) nurse put back the NGT. She had to tear off the sticky tegaderm that was supposed to keep Cohen from taking the NGT out, and when I say “tear”, that’s exactly what she did. Cohen screamed and I was close to doing the same! My eyes went wide and I was pissed at she handled it. I left crying that afternoon and prayed we wouldn’t get that nurse again.
Cohen’s diaper rash continued to be a pain in everyone’s butt (pun intenteded)! We were having to put allllllll kinds of creams and lotions and butt pastes on his little bottom at every touch time. Eventually, we started putting a pee pad in his bed, then would put Cohen on his stomach without a diaper and tape oxygen tubing to Cohen’s bed, aimed right at the rash. It was a sight! But over time, that rash finally went away!
Cohen ended up pulling out his NGT again just a few hours later. He got very good at grabbing hold of that tube when no one was watching and pulling it out!
On December 17th (17 days old), Jason’s cousin, Jancee, got to hold Cohen for the first time. This was also the first day that Cohen breastfed for 23 minutes, so he didn’t have to have a bottle or get anything through his NGT!


21-25 Days Old
Cohen is 4 lbs!! So close to our goal weight! He also got to meet Santa Clause and get pictures with him.

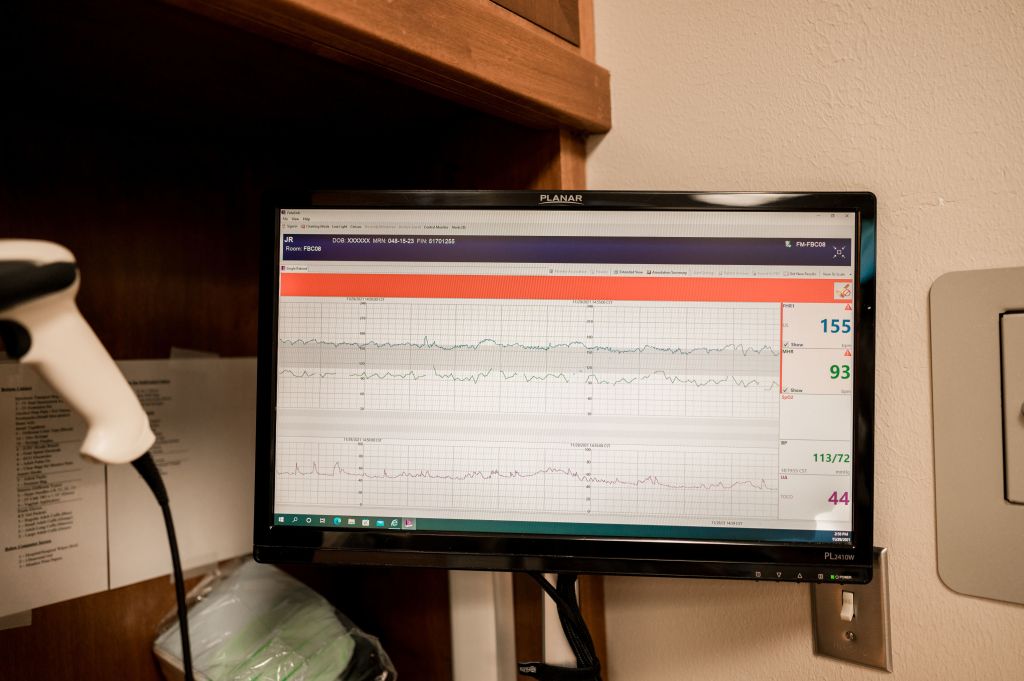
Cohen is having bradycardia (what we would call “brady’s”), which means he would have an abnormal heart rhythm and his heartbeat would slow. This had been happening for a few days now, but it started to become more of a concern because we learned he couldn’t go home unless he was “brady free” for 48 hours, and he was having several a day at this point.
One day, we showed up to a touch time and Cohen was in a swing – his nurse said she put him in “time out” because he wound’t stop crying. He was very happy in the swing though! So cute!

We spent Christmas Eve and Christmas Day in the hospital. It was extremely hard. We didn’t do Christmas with any family except for a quick “snack” on Christmas Eve with Jason’s parents and Christmas lunch with my parents and Karli. We missed seeing everyone, but we knew we didn’t want to be away from Cohen for more than was necessary. Christmas Eve, Jason and I gave Cohen a sponge bath together – he loved it! It was the first bath that I got to be a part of as his mom. Christmas Day, Cohen didn’t use his NGT at all for feeds because he nursed so well! We knew we were getting close to bringing Cohen home, but he was still having those dang brady’s!!



26-30 Days Old
Cohen was still having brady’s and I was sooooo over it!! Cohen was doing amazing with nursing – we nursed at every touch time and we rarely ever had to use the bottle or his NGT (except at night), and he was gaining weight! We started to be able to tell when Cohen would have a brady – right before he would have one, he would typically choke when nursing. I started getting so frustrated, because how were we supposed to be able to keep him from choking?! No one could tell me. So I brought it up to the NP during rounds. I was ready to take my baby home. I would also get frustrated that Cohen would nurse super well during the day, but then at night, he wouldn’t take his bottles well and that’s when we had to start using the NGT.
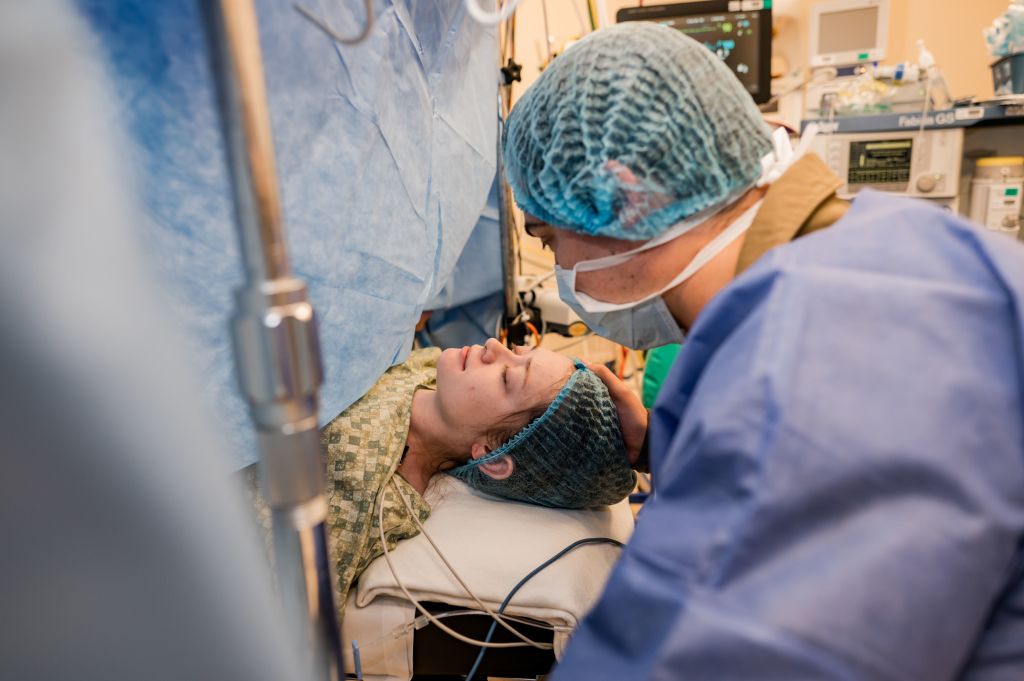
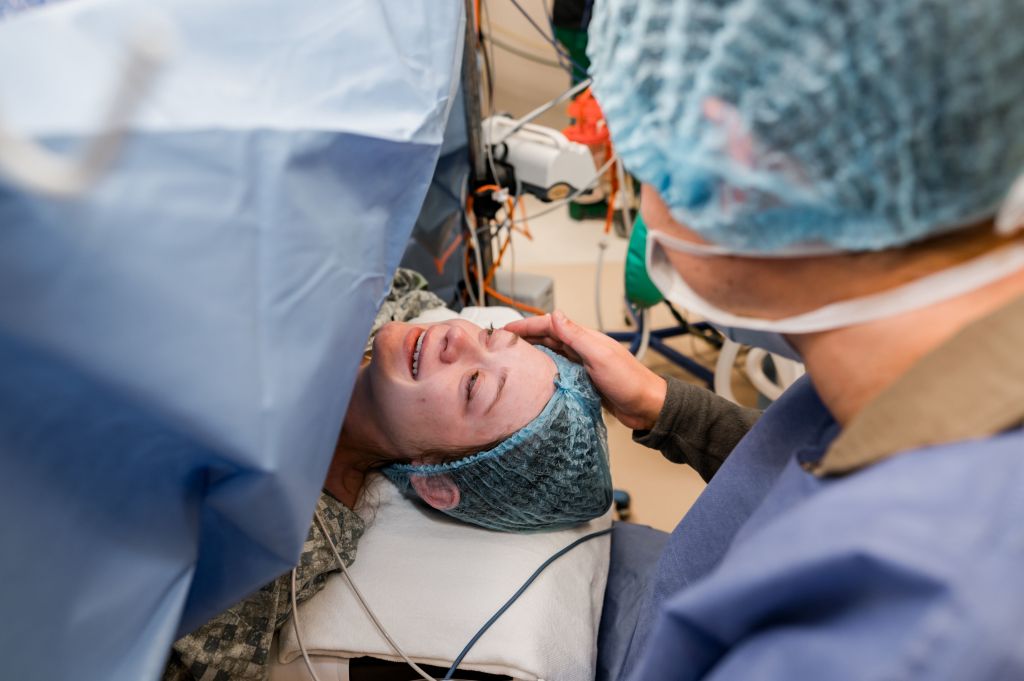
The NP asked if we wanted to “room in” for 48 hours and I said “absolutely!” So that night, Jason and I packed our bags in preparation to stay at the hospital for 48 hours so we could try to bring Cohen home. Before we left to pack up, our nurse, Gaye, put Cohen in a car seat to do a car seat test. This is where the baby has to be in the carseat for 2 hours without any bradys, oxygen issues, etc.
After showing up, prepared to room in, we went back to Cohen’s pod and as soon as we walked in, Gaye looked disappointed. She told me Cohen had just failed his carseat test, right before the 2 hour mark. I was disappointed, but knew it wouldn’t be a big deal to do another one. I was just ready to spend a full 48 hours with my baby and hopefully take him home!
Gaye, Cohen’s nurse, helped us move Cohen in one of the “room-in” rooms within the NICU. When you walk in, there is a small “foyer” with a rocking chair, sink, mini fridge and a table. You move further in and theres a queen-size hospital bed with a night stand, space for baby with all the monitors, a table, and a bathroom with a shower. The hardest part was that there were no windows. I guess it was okay from a baby standpoint, but gosh, I felt like I was in prison.


Before we were fully moved in, Cohen’s NGT was removed! We didn’t know yet, but he wouldn’t have to have it replaced at all because he was finally eating so well.

That night, Jason and I both got up every 3 hours to feed Cohen. We set alarms each time, but Cohen was actually the one who would wake us up before our alarms could. I would nurse him for as long as he wanted, then Jason would put him to sleep so I could pump. By this point, we recognized that I was an oversupplier. Honestly, my body didn’t have a choice. With Cohen not nursing well in the beginning, I had no choice but to pump in those early days. Then, when he did start to nurse well, no one told me I didn’t have to pump afterwards. I was so used to nursing then pumping – I had no idea about the whole “supply and demand” thing until my supply was already established! Looking back, I’m so thankful for the oversupply, even though it came with it’s challenges, because I never worried if I was making enough for Cohen, and I got to help nourish 14 other babies during my 15 months of breastfeeding.
But anyway, back to rooming in. We made it through our first night together as a family and I was so thankful! Unfortunately, during one of Cohen’s early morning feeds, he had had a brady, which meant we couldn’t go home for at least another 48 hours. I was devastated. Cohen, Jason and I spent the rest of the day together. Jason and I gave him another bath – just the two of us – and it was really sweet. We snuggled our baby all day and celebrated when he gained weight, considering he had been breastfeeding for the past 24 hours! Later that afternoon, the NP came by to tell us we didn’t need to stay the night again if we didn’t want to. As much as I didn’t want to leave Cohen, I knew I couldn’t spend another night in that room. I needed windows. And my own bed! We decided to go home and rest.

Jason and I decided not to come to Cohen’s 3pm touch time so we could pack and gather things up and spend some time at home. Gaye was SO excited because that meant she would get to feed him! I thought it was so sweet and loved how well she loved my baby! She actually texted me that afternoon to let me know he had taken 60mls from the bottle – 2 whole ounces! I was shocked. He had never eaten that much from the bottle before and had been struggling to take 38 mls (his minimum required)! Breastfeeding him for 36 hours proved to encourage him the most! I was so proud of Cohen.
The next day, Cohen was one month old! We resumed our normal routine with touch times, praying we would get to go home soon.

31 Days Old
Jason and I showed up to the NICU like normal – it was Friday, December 31st, so we both had the day off from work. We had a new nurse we had never had before, and when we walked in, she was bottle feeding Cohen. I immediately started to get upset because, again, our routine is for us to show up and I nurse Cohen. When she saw us though, she immediately handed him over to us, along with the bottle. She told us he had been crying and hungry! So I let it go. Then she said, “Are y’all ready to go home today?” I looked at her in shock. Then I looked at Jason. She said, “Oh, they haven’t told you yet?” We shook our heads. No, no one had told us! We didn’t think it had been 48 hours since Cohen’s last brady, and Cohen hadn’t had a carseat test yet. But, our nurse assured us that they had done a carseat test last night and he passed, and he was ready to go home! We were overjoyed! We had to wait around for a few hours until the nurse practitioner could come and discharge us. So in the meantime, we snuggled Cohen and picked up his multivitamin from the pharmacy downstairs. Jason and I decided not to tell anyone we were taking Cohen home.



Once we were finally discharged, we texted my parents and asked if we could come over for a little bit. They said yes, so we immediately went to their house with Cohen! When we got there, my mom was in her bathroom getting ready. Jason and I quietly snuck in and took Cohen out of the carseat. My dad saw us and seemed to be pretty surprised! I took Cohen and walked to my parents bathroom. When my mom saw me in the doorway, she screamed! Then she cried. It was a sweet surprise! We spend the afternoon there, letting everyone get all the Cohen snuggles in.



After dinner, we headed home and let Meredith and Leia meet Cohen – they loved him! Leia actually turned out to be pretty protective over him – it was so sweet.

Well, there you have it. The story of quite possibly the worst month of our lives! Of course, Cohen makes it all worth it.
There is a lot I can’t remember, or have probably forgotten. One thing I barely touched on was the fact that every single morning, I would come in and pray that Cohen had gained weight. It was crucial. I became obsessed with how many grams Cohen weighed that day. Not only that, but how many mls Cohen was taking from his bottle, when we were bottle feeding – and especially overnight. I let those numbers easily dictate my emotions. It was truly traumatic.
I never want to have to go back to the NICU again. Even today, walking past it at work is something I try to avoid at all costs. Before we left, our nurses asked us to bring Cohen by to visit, and I have yet to do that because it’s just too hard! All of the feelings and emotions come rushing back, and it genuinely makes me want to throw up.
If you’ve every had a baby in the NICU, where it was 1 day, 30 days, or 200 days, you are a warrior. Leaving your baby behind is the absolute worst, and it takes the strongest parents to do it! I am proud to have made it through that season, and pray I never have to go through it again. But if I do, for whatever reason, I know the Lord will sustain me and that He will be my rock and my fortress. He is who I will turn to for joy, peace and patience, because only He can provide those in the most difficult of circumstances. I am thankful for His faithfulness!
























































 I’ve been wanting to write this blog post for a few months now… but I wasn’t ready. My heart was not ready. But with the start of a new year, I’ve felt the Holy Spirit’s prompting to share.
I’ve been wanting to write this blog post for a few months now… but I wasn’t ready. My heart was not ready. But with the start of a new year, I’ve felt the Holy Spirit’s prompting to share.